Our understanding of neuropsychiatric illnesses depends heavily on human research that aims to clarify how the brain functions in health and disease. One such disorder, Epilepsy, has a considerable health burden.
Epilepsy is a chronic medical disorder that affects both patients and caretakers and is incapacitating. Seizures are caused by aberrant electrical activity in the brain in cases of Epilepsy. This abnormal electrical activity starts simultaneously from the right and the left cerebral hemispheres. Epilepsy patients have been demonstrated to have additional psychiatric comorbidities. Anxiety, depression, and psychosis are the three psychological disorders that epilepsy patients experience most frequently. EEG findings are crucial not only for diagnosing Epilepsy but also for managing the patient.
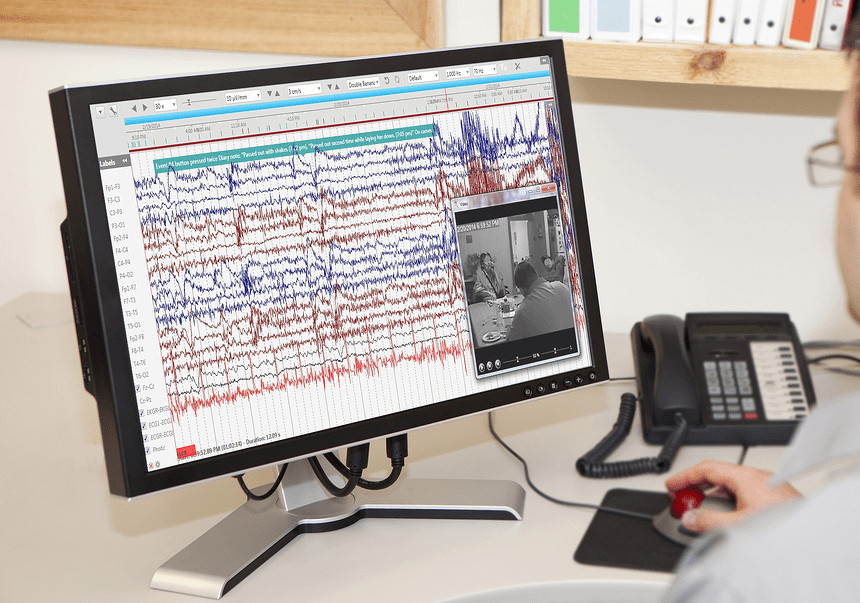
In contrast to an EEG, which records brainwaves, a video EEG (or electroencephalograph) captures what a patient is doing or experiencing on camera. When evaluating if an event is epileptic, identifying the precise seizure type for treatment choices, and locating the site of the seizure onset in patients with medication-resistant Epilepsy who may be candidates for epilepsy surgery, video EEG is the most helpful tool.
The goal is to be able to visualize what is happening during a seizure or other occurrence and contrast the image with what the EEG captures concurrently. The method simultaneously captures behavior on tape or digital video and brain activity on an EEG. The seizures or other behaviors are typically recorded, the patient is admitted to a specialized hospital ward, and the drugs are decreased or stopped.
In patients with psychosis, EEG findings may indicate the presence of a focal CNS pathology. There are few studies on the electrophysiological characteristics of patients with concurrent psychosis and Epilepsy. The complex relationship between EEG activity and neuropsychological status included positive and negative correlations at lower and higher alpha frequency sub-bands for each cognitive task. The pattern of these correlations varied depending on the particular cognitive task. Length of the psychosis, psychopathology, and presence or absence of seizures have all been used to categorize psychosis in Epilepsy.
The gold standard for the diagnosis of Epilepsy and classification of seizure type continues to be continuous video-EEG monitoring. EEG findings in patients with psychosis can be difficult to interpret. The clinical conditions of the patients largely influence these findings. Traditionally, Epilepsy has been treated with antipsychotics and benzodiazepines. For instance, benzodiazepines may reduce the number of epileptiform discharges observed on an EEG. Moreover, a single EEG may only reliably rule out a seizure disorder in about 50% of patients. Therefore, EEG in patients with psychosis should not be routinely ordered.
Psychosis in Epilepsy can take on many forms. Postictal psychosis is the most common type. This type is associated with seizures and can last anywhere from one to three days after the seizure. Its onset may be unpredictable, and the person may display psychotic symptoms at any time. Psychosis is a joint presentation in the emergency department. However, it is essential to distinguish it from other conditions to ensure the correct diagnosis and treatment. Moreover, the early identification of autoimmunity may lead to a better prognosis. For example, patients with autoimmune encephalitides may present with abnormal EEG findings, although these findings are not specific to these diseases. The EEG findings in Epilepsy with psychotic symptoms can provide a valuable biomarker of neuro-age. In addition, it may help differentiate patients with different epilepsy phenotypes, including symptomatic generalized Epilepsy (SGE)/ progressive myoclonic Epilepsy (PME) and temporal lobe epilepsy with hippocampal sclerosis (TLE-HS).
Postictal psychosis is seen in up to 9% of Temporal Lobe epilepsy patients who are having video-EEG monitoring, and it most frequently occurs in people who have bitemporal lobe dysfunction7. In epilepsy centers, video-electroencephalography monitoring is a safe way to assess patients with refractory temporal lobe epilepsy, mesial temporal sclerosis, and psychosis of Epilepsy.
References:
https://neuro.psychiatryonline.org/doi/pdf/10.1176/appi.neuropsych.11120363
https://www.hindawi.com/journals/crinm/2013/159842/
https://journals.lww.com/theneurologist/Abstract/2018/09000/Investigation_of_the_Video_EEG_Findings_and.7.aspx
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4899965/
https://www.epilepsy.com/diagnosis/eeg/video-eeg