Insulin resistance, once viewed primarily as a precursor to type 2 diabetes mellitus (T2DM), is now recognized as a multifaceted metabolic disorder with far-reaching implications beyond glucose regulation.
Among its myriad consequences, insulin resistance exerts a profound impact on renal health, contributing to the development and progression of kidney disease.
INSULIN TESTING KIT IS AVAILABLE ON CHEAP PRICE: GET NOW
In this article, we delve into the intricate interplay between insulin resistance and renal dysfunction, exploring the diverse mechanisms through which insulin resistance disrupts kidney homeostasis and highlighting the implications for clinical management.
Insulin Resistance
The insulin is produced by the pancreas, plays a central role in regulating glucose metabolism by promoting glucose uptake into cells and inhibiting hepatic glucose production.
This arises when target tissues, such as muscle, liver, and adipose tissue, exhibit reduced sensitivity to insulin action, necessitating higher insulin levels to maintain normoglycemia.
While genetics and lifestyle factors contribute to insulin resistance, obesity, physical inactivity, and dietary habits are major drivers of its prevalence.
The Ripple Effect on Kidneys
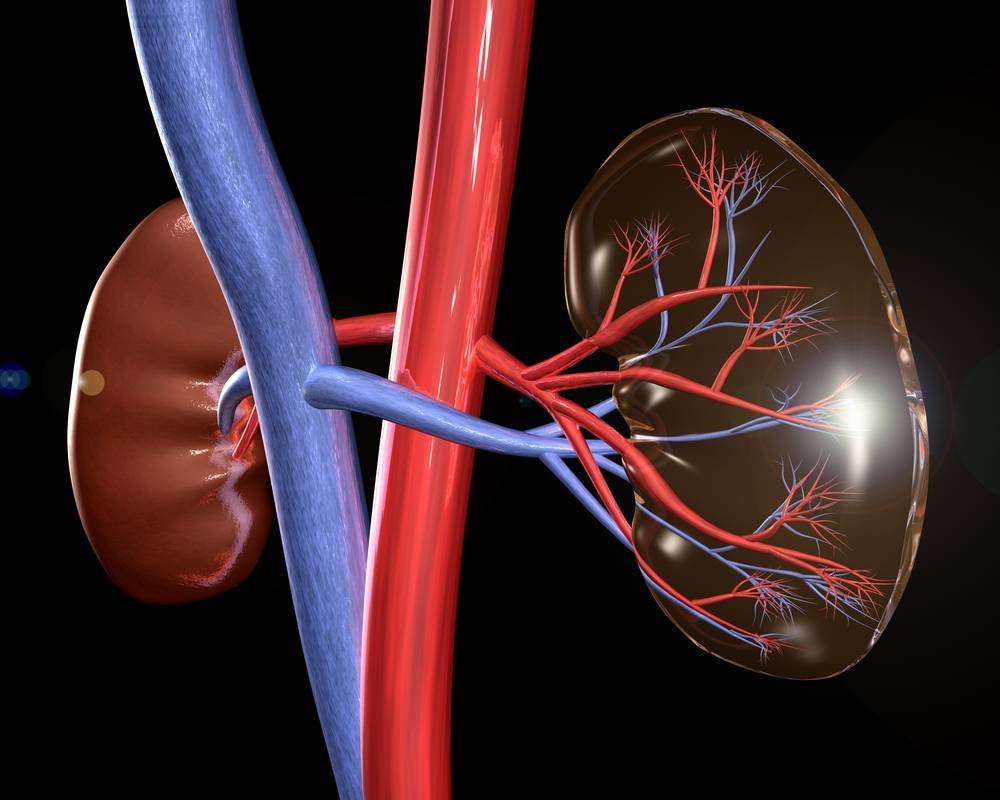
The kidneys, a sophisticated organ that are responsible for removing waste from blood while maintaining the electrolyte and fluid balance are intimately connected to systemic metabolic functions.
Insulin resistance, como revertir la resistencia a la insulina, disrupts this delicate balance, exerting a ripple effect on renal physiology through various interconnected pathways.
Hemodynamic Alterations:
Insulin resistance contributes to systemic hypertension through mechanisms involving impaired nitric oxide bioavailability, enhanced sympathetic nervous system activity, and activation of the renin-angiotensin-aldosterone system (RAAS).
Elevated blood pressure imposes hemodynamic stress on the kidneys, leading to glomerular hyperfiltration, endothelial dysfunction, and progressive renal injury. Moreover, insulin resistance-induced hypertension accelerates the progression of kidney disease, creating a vicious cycle of renal dysfunction and cardiovascular morbidity.
Inflammatory Cascade:
Chronic low-grade inflammation is the sign of insulin resistance, and is a major factor in the onset of kidney disease. Adipose tissue, especially visceral adipose tissue serves as a reservoir of pro-inflammatory cytokines such as tumor necrosis factor alpha (TNF-a) as well as interleukin-6 (IL-6) which are known to cause kidney inflammation and fibrosis.
Additionally, insulin resistance activates toll-like receptor signaling pathways in renal cells, further exacerbating inflammatory responses and contributing to tubulointerstitial damage.
Dyslipidemia and Lipotoxicity:
Insulin resistance is closely linked to dyslipidemia. It is characterized by an increase in triglycerides, cholesterol from low density lipoprotein (LDL-C) and lower levels of cholesterol from high density lipoprotein (HDL-C).
Dyslipidemia promotes the accumulation of lipid deposits within renal cells, triggering oxidative stress, mitochondrial dysfunction, and apoptosis. The phenomenon, referred to as lipotoxicity, impedes kidney function and accelerates the development of kidney disease especially in conjunction with metabolic syndrome and obesity.
Renal Insulin Signaling:
The kidneys themselves are targets of insulin action, expressing insulin receptors and signaling molecules involved in glucose uptake, sodium reabsorption, and vascular tone regulation.
Insulin resistance disrupts renal insulin signaling pathways, impairing sodium handling, promoting sodium retention, and contributing to volume expansion and hypertension.
Furthermore, dysregulated renal insulin signaling exacerbates glomerular hyperfiltration and promotes the development of albuminuria, early markers of kidney dysfunction.
Clinical Implications and Management Strategies
Given the complex interplay between insulin resistance and kidney health, clinicians face the challenge of managing these intertwined metabolic and renal abnormalities effectively. A comprehensive approach encompassing lifestyle modifications, pharmacotherapy, and targeted interventions is essential to mitigate the deleterious effects of insulin resistance on the kidneys.
Lifestyle Modifications:
Encouraging individuals with insulin resistance to adopt healthy lifestyle habits, including regular physical activity, balanced nutrition, and weight management, is paramount. Exercise improves insulin sensitivity, reduces inflammation, and lowers blood pressure, thereby ameliorating renal dysfunction and reducing cardiovascular risk.
Interventions for diet, like the Mediterranean diet, or the Dietary Approaches for Stopping Hypertension (DASH) eating plan, focus on whole food, fruits, vegetables, healthy proteins that promote healthy metabolism and kidney function.
Pharmacotherapy:
Pharmacological agents targeting insulin resistance and its associated comorbidities play a crucial role in managing kidney issues in insulin-resistant individuals. Metformin, an insulin-sensitizing agent, remains a first-line therapy for T2DM and insulin resistance, offering renal protective effects through mechanisms involving AMP-activated protein kinase (AMPK) activation and anti-inflammatory actions.
Sodium-glucose cotransporter 2 (SGLT2) inhibitors and glucagon-like peptide-1 receptor agonists (GLP-1 RAs) demonstrate renoprotective benefits beyond glycemic control, including reductions in albuminuria, preservation of glomerular filtration rate, and attenuation of cardiovascular events.
Blood Pressure Control:
A shrewd approach to managing blood pressure is essential in halting the progress of kidney disease as well as reducing risks to cardiovascular health in individuals with insulin resistance. Angiotensin-converting enzyme inhibitors or ACE inhibitors and angiotensin II receptor blockers (ARBs) are preferred agents due to their renoprotective effects and ability to mitigate proteinuria. Combination therapy with calcium channel blockers, diuretics, or mineralocorticoid receptor antagonists may be necessary to achieve target blood pressure goals and optimize renal outcomes.
Lipid Management:
Addressing dyslipidemia is essential in managing kidney issues in insulin-resistant individuals, given its role in promoting atherosclerosis and renal injury. Statins and HMG-CoA reductase inhibitors, are recommended as first-line therapy for dyslipidemia in individuals at high cardiovascular risk, including those with insulin resistance and kidney disease.
These agents lower LDL-C levels, stabilize atherosclerotic plaques, and exert anti-inflammatory effects, thereby reducing the risk of cardiovascular events and preserving renal function.
Insulin resistance’s ripple effect on kidneys underscores the intricate interplay between metabolic and renal pathways. This necessitates a holistic approach to management.
By addressing underlying metabolic abnormalities, controlling blood pressure. Also, optimizing lipid profiles, and implementing lifestyle modifications, clinicians can mitigate renal injury and improve outcomes in insulin-resistant individuals.
Collaborative efforts between primary care providers, endocrinologists, nephrologists, and allied health professionals are essential to tailor interventions to individual patient needs and maximize the efficacy of therapeutic strategies.
Emphasizing patient education, regular monitoring, and early intervention are key pillars of effective management, offering hope for improved renal health and enhanced quality of life in this vulnerable population.